And just like that, three months – more! – have passed. My first rotation here in Auckland came to an end just a couple of weeks ago. So many feelings! I’m now in a new hospital (still in the city), doing a completely different specialty. And settled enough to have started enjoying it! It’s all going way too fast.


I wanted to take a moment to write a little about work over the past few months. While everything is still fresh, to keep a record of the details that seem important right now, because I know with time the focus will shift.
Heads up: it might get long.

“Like rounding with The Reaper,” is how my reg summed up a particularly difficult stretch on the ward a month or so ago. It felt relentless. Morning rounds heavy with impossible conversations, afternoons under fire from teams with conflicting priorities, family meeting after family meeting, death upon death upon death.
I can’t tell you what it is to know that you are so close to death. But I can tell you what it is to look into a man’s face and see playing out across it that struggle between the deep certain knowledge: that it is over, and the most basic of human instincts: the fight to live. I have seen what it is to watch the features of a woman change as she is told she must die, the shock in the eyes, the squaring of the jaw, and that sudden wave of nausea, a punch to the guts. I have seen what it is for a man try to answer that question: do you want to continue? The words are on the tip of his tongue, he can’t get them out. Arrived at the very edge of life, wanting to let go, not quite able to let go. The world’s deepest, longest, saddest sigh.
Let me tell you what it is like to be present in a room where a husband and wife fight over his life, where she sobs and begs him to continue his life-sustaining treatment, as grown children watch silent in grief: he stares straight ahead, his face white with pain, wet with tears, and tells us that he can’t. I leave these patients with hands cold as ice, cheeks flushed and throat aching, only to walk on into the next room with a smile, to pick up the next job, to go get coffee. All of the emotions are there: sadness, pity, sympathy, anger.
It takes an excellent physician to have these conversations, to navigate them, to take responsibility for the decision to withdraw treatment when it is evident that no one else can. Oh but I have seen incredible medicine over the past few months.
I wasn’t sure what to expect before starting. As I wrote back in September, the first few weeks were a blur of new systems, endless questions, a constant nagging feeling of anxiety, frustration, incompetence. Not for lack of support – I couldn’t have asked for a better team of ward staff to work with. But after a few years of work you begin to hold yourself to your own standards. It was difficult to feel every day that I was falling short.
What helped the most during those early days were the one-on-one moments with patients. Taking bloods, placing a cannula for an intravenous drip, reviewing someone who was unwell out of hours. I know some people get bored of these relatively mundane jobs. But they created little pockets of something almost akin to mindfulness in my day: for a few brief minutes my attention would be wholly focused on the task at hand and the person in front of me. I make conversation always as I go – real conversation, not just small talk – and it would give me a break from my own internal criticism, forcing my mind back to what really mattered, pushing everything into perspective.
“You should be a nurse”, one of the patients that I saw during of these out-of-hour reviews told me, in the middle of one of those busy shifts where your phone doesn’t stop going off and your list of jobs seems to grow ever longer. “You’re so gentle”.
While I was putting a line in and taking blood cultures I told her how I had come across from the UK, how long and awful the flight was, and we talked about my sisters in Paris and the Netherlands, my brother in London, how rarely we all get together these days. I told her I’m not planning on being here forever, but that you never know what’s going to come up. “Oh no”, she cried out, genuinely upset. “You must go home, your poor mother will miss you ever so much, please tell me you’ll go home”.

One thing to get used to was the change of pace. The on-call shifts I worked – a mix of ward cover and medical clerking – were pretty busy. The long days are reallly long: from 8am til 10.30pm if you’re working a medical specialty (often from 6.30am or 7am til 10.30pm if you’re doing something surgical).
Nights are shorter to make up for it, just 10pm til 8am, which is kinda nice, but they are only just beginning to introduce the concept of sleep recuperation days that we have now in the UK. In Middlemore they split the week 5:2. So you would work Sun-Mon-Tues-Weds-Thurs night, finishing on Friday morning, and have Sat/Sun off before starting back on Monday. Or you’d work a normal week Monday to Thursday, have Friday day-time off and work Fri-Sat night, finishing on Sunday morning, and would then be back onto day shifts again on Monday.
I worked about one in three weekends, and I had a whole bunch of twelve day stretches in my rota, every single one of them finishing with a long day on the last day, which was pretty exhausting. By the time it got to around 8pm on that 12th day I would be just about done caring about anything or anyone any longer… it really was pushing you to the very edge of burnout. You don’t get any kind of zero days after those, either.
So I think the rota I was working was relatively tough, although pretty similar to some of the ones I worked back in the UK. All of my leave requests were rejected, so I didn’t get a break. But I’ve enjoyed the work so much that I honestly haven’t minded. And although a lot of the day to day ward work was emotionally draining, the volume was nowhere near comparable to what I was used to back home.
When I spoke to my sister the other day she asked me if ever get tired any more. “You were always tired last year whenever we saw you, whenever we talked”.
The answer is yes, of course I have been tired, I often am. But it’s a different kind of tiredness, a very physical kind of exhaustion. The shifts are too long, but give me a night to sleep and I’m ready to go again. After a weekend off I’m relatively refreshed. The tiredness I had in the UK ran much deeper. It was the sheer volume of shit that you saw, terrible deaths, such unhappy lives, and so many so often that you scarcely had time to process them until much later on. My experience of that has been different here.

Renal is not a light-hearted specialty.
Many of the patients are nearing the end of their life. Those that are on renal replacement therapy are living on borrowed time, and on such a short leash, forced to stay within range of their dialysis machine at all times, completely robbed of any independence or freedom. The mechanical filtration that we are able to offer removes things from their blood that would rapidly kill them, but is unable to replace the many roles that a healthy kidney fulfills. They live with skin that is permanently itchy and dry, a thirst that they can never quench, hair brittle and thin. Their bodies are ravaged by our attempts to gain intravenous access, arms disfigured with bulging dysfunctional fistulas, vessels narrowed and tortuous, skin scarred and tight. Their hearts are giving up on them, their lungs are constantly heavy with water, they are always fighting off some or other infection. All of their energy is consumed by the battle to stay alive.
Renal failure can strike anyone out of the blue: an unlucky consequence of a simple throat infection. It can be part of devastatingly bigger picture, a body under attack from within, perhaps even the least of that person’s problems. It can be something you have the bad luck to be born into, an unfortunate genetic combination that dictates the rest of your life. It can be something supposedly brought upon yourself, the consequence of many years of bad health: high blood pressure, poorly controlled diabetes, things which could theoretically have been prevented. The failure to prevent them invariably belongs to us all. It is a failure of society, a failure to offer infrastructure, support, education and hope, and yet we often find it easier to judge and blame these people, to our shame.
The best possible option for someone with end-stage renal failure is to offer them a kidney transplant, which is a miraculous feat of surgery and medicine. And yet even those who are lucky enough to receive one will never live the carefree life you and I know. They exist in constant immunosuppression, we beat back their body’s defence system so that it doesn’t reject the foreign kidney that we have put inside them, but with the side effect that it is also unable to fight any infections they catch, unable to stop the spread of cancers. The drugs we give them are coarse, sometimes with particularly unpleasant side effects. They live forever under the looming shadow of rejection.
Given that most patients with renal failure will never recover, and those with transplants will need to be monitored for life, there is a lot of continuity of care, which can be both a blessing and a curse. Being forced into a medicalised life can do strange things to some people, distorting their need for attention, causing them to act in ways that provoke infinite exasperation. Some people are never quite able to accept the restrictions that the diagnosis places upon their freedom. They live in constant self-induced tortuous discomfort, pushing their bodies to very edge, almost willing them to break. I don’t feel that we are in any position whatsoever to judge such patients, so terrible is their lot, but even so they induce so much disappointment and frustration. Of course, there are always perfect patients, who live exactly as we dictate, and have good enough luck to do relatively well. But those are the ones you see comparatively little, those aren’t the patients who make regular appearances on your ward.
This kind of patient group is pretty polarising. Some doctors have no time for the antics, no patience for the renegades, for those who seem bent on self-sabotage despite our best efforts. Others shake their heads in despair, but have respect or affection enough to cope.

Personally, I find the pathology of renal medicine fascinating. It is an area in which our understanding of certain things is incredibly basic, the tools which we have at our disposal to try treat are incredibly crude. There is a lot of scope for research, discoveries, improvement.
I don’t necessarily find it easy to deal with the things I have been writing about. But I do find that the more difficult things are often those that ultimately prove most rewarding. There is something very humbling about working in such circumstances, it stops you from taking for granted your own good fortune, it’s a constant reminder to live well.
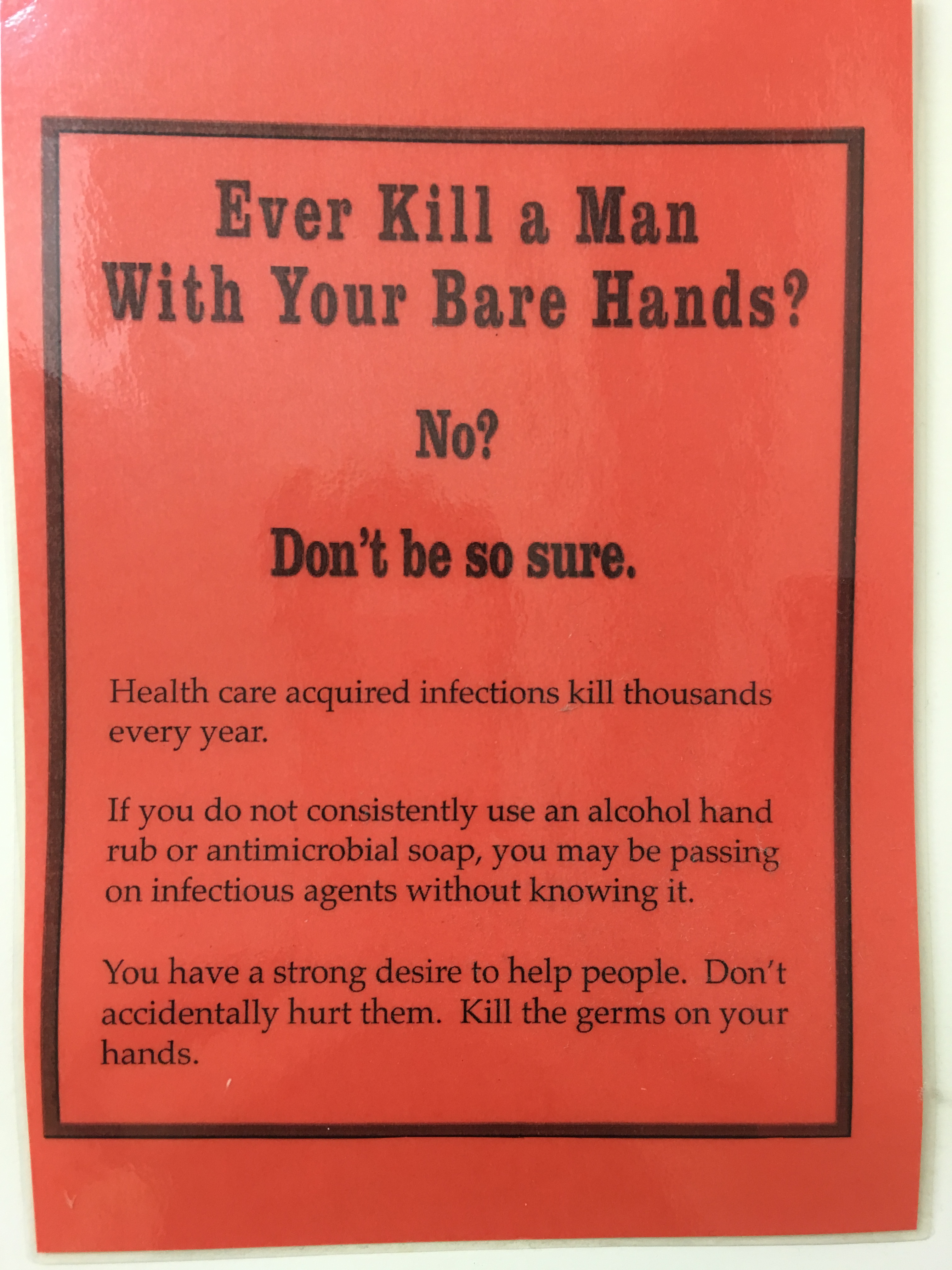
I enjoyed my renal placement more than I can say. I loved the medicine and the patients, I loved their character, and the stories they had to tell. I had the good fortune to work with an excellent team of nurses and allied health professionals, the best “offsider” you could get, incredibly supportive registrars, very good consultants. I had more coffee breaks than I would ever have imagined possible, certainly for someone who doesn’t drink coffee, and will be forever indebted to them for the wisdom, laughter, tales that were imparted. I grew crazy fond of Middlemore, with its unruly poster-makers, hopelessly incompetent RMO unit, rooms overflowing with Whanau, corridors lined with stalls straight out of a farmer’s market, selling vegetable spiralisers, beeswax candles and stockings. I loved the constant buzz of beautiful singsong Island languages, my daily chats with the cafeteria ladies, the automatic bond formed with everyone who’d fallen victim to the flea-infested RMO lounge.
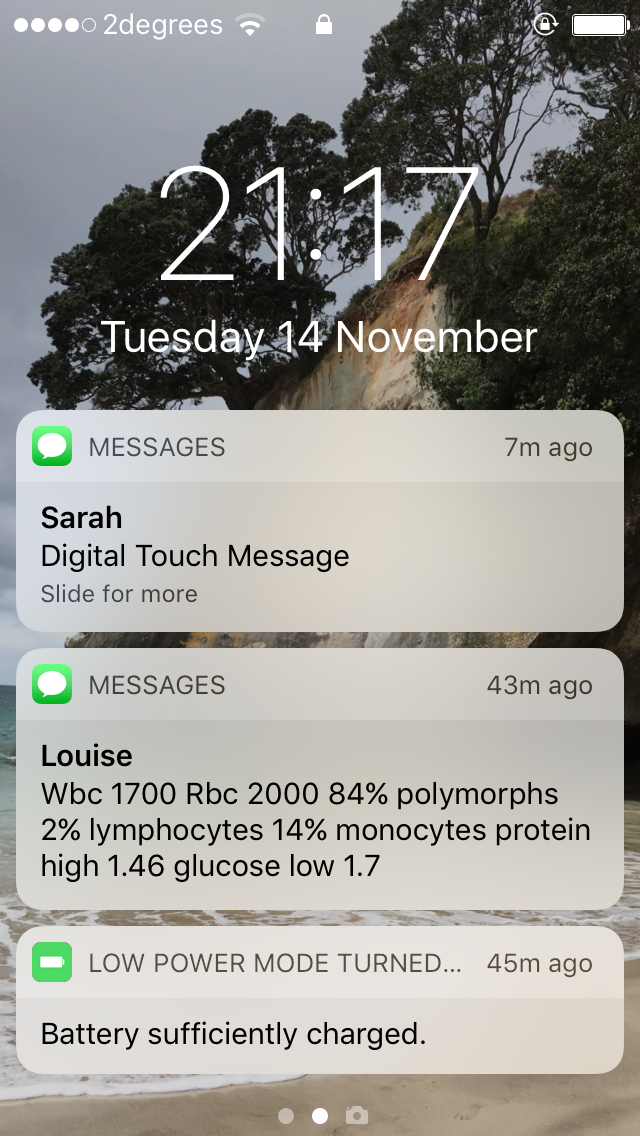
We treated meningitis and encephalitis, necrotising fasciitis, countless cases of peritonitis, fluid overload, electrolyte imbalances and arrhythmias. There were plenty of acute coronary syndromes, strokes, hypertensive emergencies. Lots of new diagnoses of renal failure, some amyloidosis, some vasculitis. We cared for pregnant ladies with Lupus, teenagers with heart failure, diabetics with HbA1cs over 150. We (unintentionally) gave people C Dif on more than one occasion, and came very close to spreading norovirus round the dialysis unit.
I saw the aftermath of disseminated septic arthritis, the diagnosis of calciphylaxis, almost all the different cranial nerve palsies and plenty more neurology besides. I learnt how to manage an acutely thrombosed fistula. I watched the most skillfully managed family meeting, I witnessed many ways to approach palliation. I listened in on weekly conversations with the infectious diseases team, maybe even learnt a thing or two. I was able to do a number of lumbar punctures, ascitic taps and drains, even a chest drain. I had a ton more practice doing cannulas. I am most likely colonised forever with MRSA, ESBL, VRE.
I’ve gotten a surprising amount of questioning about the choices that I made in coming here, the choices that I am making in continuing to work at a house officer level, instead of stepping up as a registrar (which is expected of you here as a PGY3). It is all entirely well-meant, although I feel there is a lot also of people (perhaps subconsciously) trying to herd you back onto the “right” track, put you back in the box. One thing I will say: it takes strength to resist that, to say no, actually, I know what I need to be doing right now and that is not it. But I didn’t come half way across the world just to slot into another system. I’m forging my own path out here, learning from my own mistakes.
I’m not ready yet to commit to specialty training. I’m still figuring out what will work best for me. But I have two cornerstones when it comes to my career. One is knowing the kind of person I want to be. The other is an almost ineffable sense of what I need to be doing to get there.
No part of medical sciences came naturally to me. Not biochemistry, not physiology, not statistics. Other parts of medical practice do: kindness, empathy, compassion. An instinctive understanding of human urges and motivations. The stubborn determination needed to become good at venepuncture, cannulating, practical procedures. “Soft” skills. But perhaps also the ones that are hardest to teach.
I’m okay with that. It might take me ten times longer to understand a concept than it would somebody more scientifically minded, but if that’s how long it takes then that’s how long I’ll spend on it. I want so badly to be good. It drives me into the small hours of the morning, it wakes me before sunrise with a fire in my belly. For so long now I have had such a clear image in my mind of the kind of doctor I aspire to be. I try so hard every day, and I know that it’s as much about the journey as the destination, that it couldn’t happen without all of these lessons along the way, but ahhh sometimes my heart aches so much just longing to be that person already.


One day I will be.
In the meantime, just trying to lean into this season of life with patience and grace.
A final observation.
Perhaps it’s something to do with being stripped of basic day-to-day familiarity out here, or perhaps it’s just to do with being so far from home, but certain scents, colours, temperatures bring me back memories these days with a rush so hard it is overpowering.
All of a sudden I am eight again, my tongue is stained purple with cherries and the sun is hot on my mosquito-poxed skin and I just am, neither happy nor unhappy. Next I’m fourteen, my brother and I are sucked under powerful waves, off the Costa del Sol. I let go of his hand, but we make it out, and when we get home there are millions of tiny twirled shells in our clothes. I’m three, sat on my Dad’s lap, reading from a book, troubled by the fate of the protagonists, invested in their wellbeing. Now I’m a teenager and laughing in French, bored in the classroom, drawing on friends’ notes, waiting for the bell to ring. I’m running down dusty streets panting; I’m ten, cupping my hands at a water fountain and drinking greedily so I can get back onto the court.
I’m twenty and laying in the grass as the evening sun shines through the pines surrounding a sports field in Germany, while co-workers cook bolognese on a stove outside, and we argue about spaghetti and noodles and I tell everyone I don’t think I will ever be more happy than in this moment right now. I’m twenty seven and watching the pink skies out of my flat window pre-night shift, blasting the dog days, utterly at peace. I’m eighteen and lying under the trees leading to Trinity Backs with my boyfriend, still a child, talking about burying pots of gold in all places we’ve been happy.
One after another, they bubble up, spill over. Every day something will prompt a recollection of a moment I hadn’t thought about in years. The effect is strange, though not unpleasant. It is almost like being stripped down to my core, a constant reminder of the things that have made me who I am. But it gives me a certain strength, and I’m glad of it, especially on those days where I feel lost and confused.

Over and out.
Love to you guys as always.
Zx